Actinomycosis: Causes, Symptoms, & Treatment - What You Need To Know
Could a seemingly innocuous bacterium lurking in your nose and throat unleash a cascade of chronic, debilitating symptoms? Actinomycosis, a rare and often misunderstood bacterial infection, can indeed transform from a subtle presence to a formidable threat, impacting various parts of the body and demanding prompt medical attention.
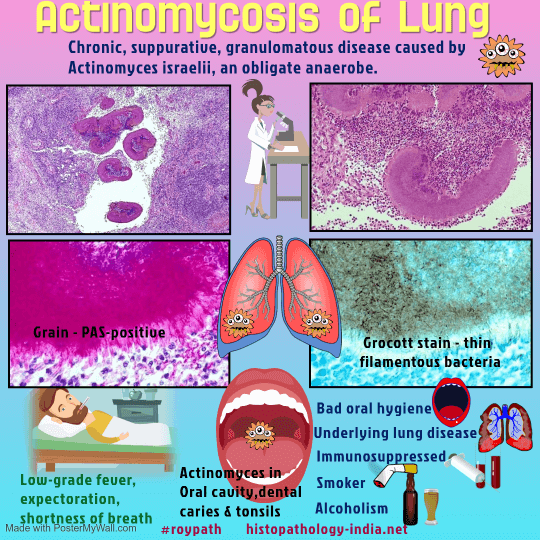
Actinomycosis, a chronic, suppurative, and granulomatous illness, is a condition where symptoms may take weeks or even months to manifest after the initial infection takes hold. While it's a relatively uncommon disease, its potential severity warrants a deep understanding of its nature, causes, symptoms, and available treatments. The bacterium Actinomyces israelii is frequently implicated as the cause, with the organism's typical habitat being the nose and throat. Under normal circumstances, these bacteria coexist harmlessly within the body; however, under specific circumstances, they can trigger a complex inflammatory process.
Actinomycosis typically finds its origin in the oral cavity and pharynx, and infections can extend to the GI tract (distal esophagus) and the GU tract. The infection can advance through various tissue planes, disregarding typical anatomical barriers. The progression of the infection and the duration of symptoms are major factors in the assessment of the disease. The nature of the infection is such that it can affect diverse areas within the body, making swift diagnosis and tailored treatment plans crucial.
Here's a glimpse into the key aspects of Actinomycosis:
| Aspect | Details |
|---|---|
| Definition | A rare, chronic bacterial infection characterized by the formation of abscesses and the development of sinus tracts. |
| Causative Agent | Primarily caused by Actinomyces israelii, a bacterium commonly found in the nose and throat. Other species of Actinomyces and related bacteria (like Streptomyces somaliensis and Propionibacterium) can also be involved. |
| Common Locations |
|
| Transmission | Actinomyces bacteria normally reside on mucosal surfaces. Infection occurs when these bacteria gain access to deeper tissues, often through breaks in the mucosal barrier caused by:
|
| Symptoms | Symptoms vary depending on the location of the infection:
|
| Diagnosis |
|
| Treatment |
|
| Prognosis | With timely diagnosis and treatment, the prognosis is generally good. However, recovery can take time, and prolonged antibiotic courses are often necessary. |
Reference: National Center for Biotechnology Information (NCBI)
Actinomycosis is a chronic localized or hematogenous anaerobic infection, often caused by Actinomyces israelii and other Actinomyces species. The bacteria, which often reside on mucosal surfaces, gain access to deeper tissues via surgical procedures, trauma, or disruptions of the mucosal barrier. The primary niche for these bacteria is the oral cavity and pharynx, but they can also be found in the GI tract (distal esophagus) and GU tract. Infections may advance through various tissue planes without respecting anatomical barriers.
Doctors often consider actinomycosis in patients who have abscesses, scar tissue, and fistulas, which may be suggestive of the disease. To confirm a diagnosis, doctors will typically obtain samples of sputum, pus, or tissue to check for various species of Actinomyces, such as Actinomyces israelii. Often, a needle is inserted through the skin to take a sample from an abscess or infected tissue. Laboratory identification is a crucial part of diagnosing the condition and is made by the appearance of the infection along with other clinical signs.
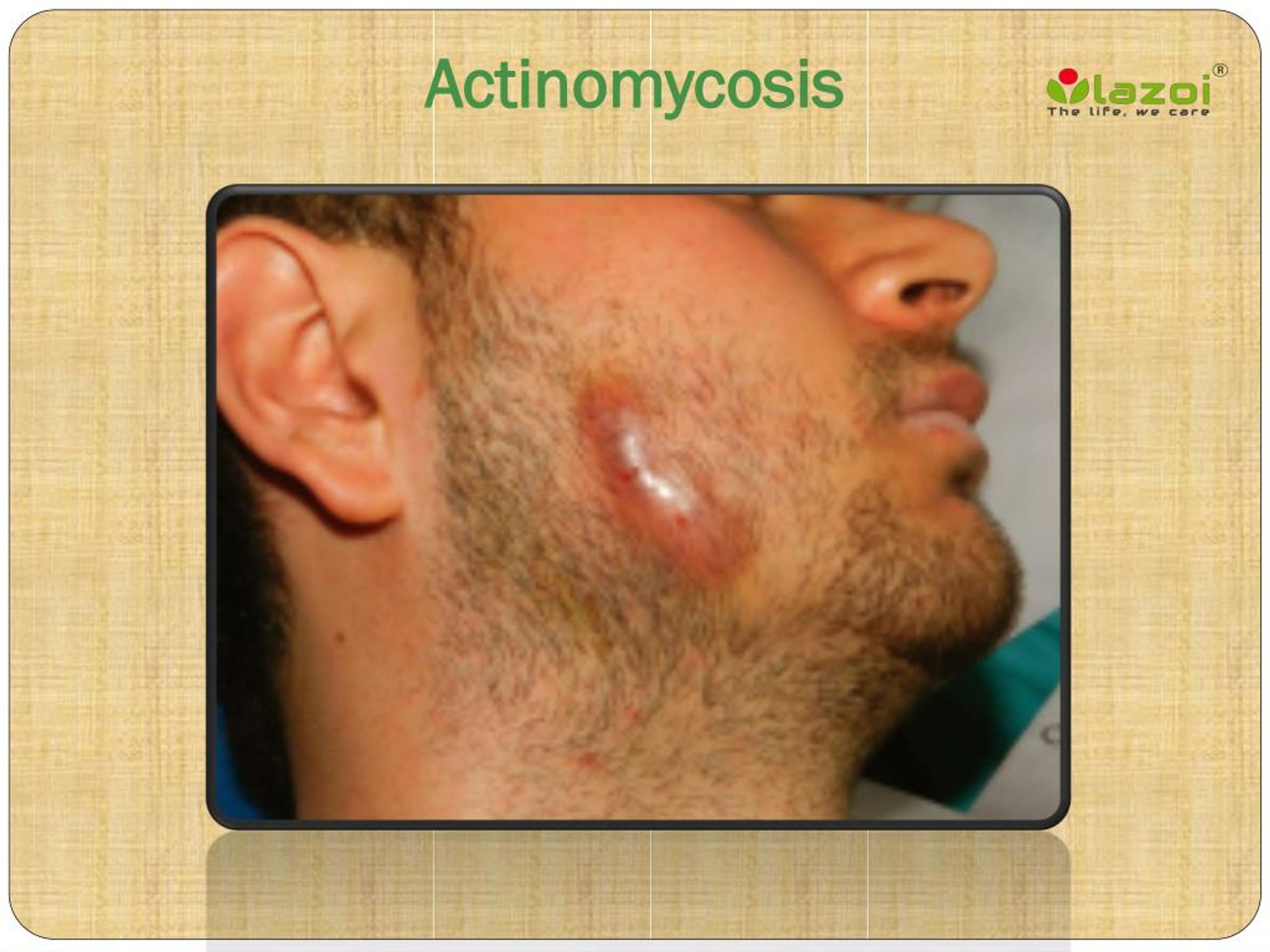
The disease is often identified by the typical appearance of the infection, along with laboratory identification of the bacteria. The chronic form of the infection is characterized by multiple abscesses that form sinus tracts, frequently associated with sulfur granules. Pain, while not always present, can arise along with the inflammation of soft tissues, especially those in the submandibular or perimandibular areas.
The symptoms of actinomycosis vary depending on the location of the infection, but some common presentations include the cervicofacial form, which is often referred to as "lumpy jaw." In many cases, this form is not accompanied by pain, but swelling and abscess formation are typical. Thoracic actinomycosis may present with symptoms similar to pneumonia or lung abscesses. Abdominal actinomycosis can manifest as abdominal pain, abscesses, and fistulas. Pelvic actinomycosis is less common and can mimic other pelvic infections, including certain cancers.
The infection is usually granulomatous and suppurative, with the chronic form resulting in multiple abscesses and the formation of sinus tracts. These tracts are often associated with sulfur granules, which can be visualized in the pus. Although pelvic actinomycosis is rare, accounting for a small percentage of all human actinomycosis cases, it can mimic various other conditions, including malignant pelvic tumors, tuberculosis, or nocardiosis. Given the variety of potential presentations, the disease can be difficult to diagnose without a thorough examination and laboratory testing.
Treatment of actinomycosis usually begins with antibiotics, starting in the hospital with intravenous administration. Patients are then often transitioned to oral antibiotics for several months, even after symptoms improve, to ensure complete eradication of the infection. Surgical intervention might also be required for more complicated cases, such as when infections occur in critical spaces or when extensive abscesses and fistulous tracts are present. It is important to complete the entire course of antibiotics as prescribed, even if symptoms resolve, to prevent a recurrence.
Prolonged courses of antimicrobials are often needed in the management of actinomycosis. Surgical intervention might be necessary in some more complicated cases, such as infections in critical spaces, for patients with severe bleeding, or when extensive abscesses and fistulous tracts are present. The main goal of treatment is to eradicate the infecting bacteria and address the inflammatory responses that the infection triggers.
Actinomycetes often invade the body through microfissures. The most common clinical form of actinomycosis is cervicofacial, often occurring after oral surgery or due to poor dental hygiene. The bacteria responsible for the infection are usually Actinomyces israelii, a common organism found in the nose and throat, where it usually does not cause disease. The bacteria can invade the body through a mechanical wound. Once it has entered the body, the infection can advance through tissue planes with no respect for anatomical barriers.
Actinomycosis is treated with antibiotics, and the initial treatment often starts with antibiotics administered directly into a vein (intravenously) in the hospital setting. Once the patient's condition improves sufficiently, they may transition to antibiotic tablets to be taken for a few months. Maintaining compliance with the prescribed antibiotic regimen until completion is very important, even when symptoms have resolved. The goal of treatment is to eliminate the infecting bacteria, control the associated inflammatory response, and prevent complications.
Because the bacteria that cause actinomycosis are typically found in the nose and throat, the infection most frequently affects the face and neck. The disease can be diagnosed by the history of the wound and clinical signs. Symptoms of pulmonary actinomycosis can be similar to those of other conditions, so doctors might need to perform several tests to confirm the diagnosis. Although pelvic actinomycosis infections are most often attributed to IUD use, other factors may contribute to the disease's presentation.
Actinomycosis can affect various organs and tissues in the human body, often manifesting with draining sinuses, abscess formation, and fibrosis. The causal agent, Actinomyces bovis, is usually present in the soil, the oral cavity of a healthy animal, pastures, and farm premises. The disease can be diagnosed by the history of the wound and clinical signs. Its symptomatology can imitate some malignant pelvic tumors, tuberculosis, or nocardiosis, which causes abscesses and fistulas. The disease can be cured by proper treatment and management.
In summary, actinomycosis is a rare but serious bacterial infection, typically caused by Actinomyces israelii. It affects various parts of the body, with the face and neck being the most common sites. Symptoms depend on the site of the infection and can include abscesses, swelling, and draining sinuses. The disease is diagnosed based on clinical findings and laboratory identification of the bacteria. Effective treatment involves prolonged courses of antibiotics, with surgical intervention sometimes needed for complicated cases. Early diagnosis and treatment are crucial to prevent serious complications and ensure a full recovery. The key to tackling the disease lies in its recognition, correct diagnosis, and thorough and consistent medical intervention.